- Home
- >
- Bipolar Disorder
Understanding Bipolar Disorder: More Than Just Mood Swings
Bipolar disorder (also called manic-depressive illness) is a mental health condition marked by extreme mood swings that go beyond normal ups and downs. These shifts in mood, energy, and activity levels can be intense and unpredictable, significantly affecting daily life, relationships, and work.
Different types, distinct experiences, shared need for care
Characterised by manic episodes lasting at least seven days or manic symptoms severe enough to require immediate hospital care. Depressive episodes typically last at least two weeks. Mixed episodes (symptoms of both mania and Major Depressive Disorder (MDD)) can also occur.
Defined by a pattern of depressive episodes and hypomanic episodes (less severe than full-blown manic episodes), but without the extreme manic episodes seen in Bipolar I.
Involves periods of hypomanic symptoms and depressive symptoms lasting for at least two years (one year in children and adolescents), though the symptoms do not meet the full criteria for hypomanic or depressive episodes.
Include bipolar disorder symptoms that don’t match the categories above but still involve significant mood changes.
An interactive infographic explaining bipolar disorder symptoms, types, and treatment options through clear visuals and easy-to-understand information
Recognising the Signs and Symptoms
| Manic Episode Symptoms: | Depressive Episode Symptoms: |
|---|---|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
Mixed Episode Features:
Some individuals experience symptoms of both mania and Major Depressive Disorder (MDD) simultaneously, which can be particularly distressing and require immediate professional attention.
The exact causes of bipolar disorder are not fully understood, but research
suggests a complex interplay of several factors:
Genetic Factors
Bipolar disorder tends to run in families, indicating a strong genetic component. If a parent or sibling has bipolar disorder, you have a higher risk of developing it. However, having a family history doesn’t guarantee a person will develop the condition, and many people with bipolar disorder have no family history of the illness.
Neurobiological Factors
Studies have shown differences in brain structure, activity,
and neurotransmitter systems in people with bipolar disorder compared to those without the condition. Imbalances in chemicals like serotonin, norepinephrine, and dopamine play a crucial role in mood regulation.
While genetic and biological factors create a vulnerability, environmental stressors can trigger mood episodes:
Diagnosing bipolar disorder requires a thorough clinical evaluation by a qualified mental health professional. At Parth Hospital, our diagnostic process includes:
Detailed Psychiatric Assessment
We conduct comprehensive interviews to understand your symptom patterns, family history, life circumstances, and conduct thorough evaluations of your mental state.
Medical Evaluation
Physical examination and laboratory tests to rule out other medical conditions that may mimic bipolar symptoms, such as thyroid disorders or neurological conditions.
Mood Charting & Monitoring
We may ask you to track your moods, sleep patterns, energy levels, and other symptoms over time to identify patterns and triggers in your condition.
Collateral Information & Assessment Tools
With your permission, we speak with family members or close friends to gain additional insights, and use validated psychiatric rating scales to assess symptom severity.
Medication Management
Medications form an essential component of bipolar disorder treatment. Our experienced psychiatrists carefully select and monitor medications to manage symptoms effectively while minimising side effects.
Common medication categories include:
- Mood Stabilisers: Lithium, valproate, carbamazepine, lamotrigine
- Atypical Antipsychotics: Quetiapine, olanzapine, aripiprazole, risperidone
- Long-Acting Injectable Antipsychotics (LAIs): For improved medication adherence and stability
- Adjunctive Treatments: Carefully prescribed as needed
The specific medication regimen is individualised based on your symptoms, medical history, and treatment response. We emphasise medication adherence and provide thorough education about your treatment.

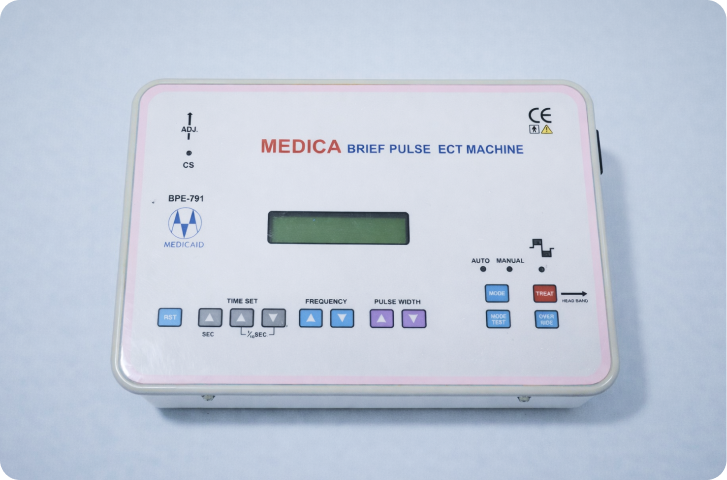
Electroconvulsive Therapy (ECT)
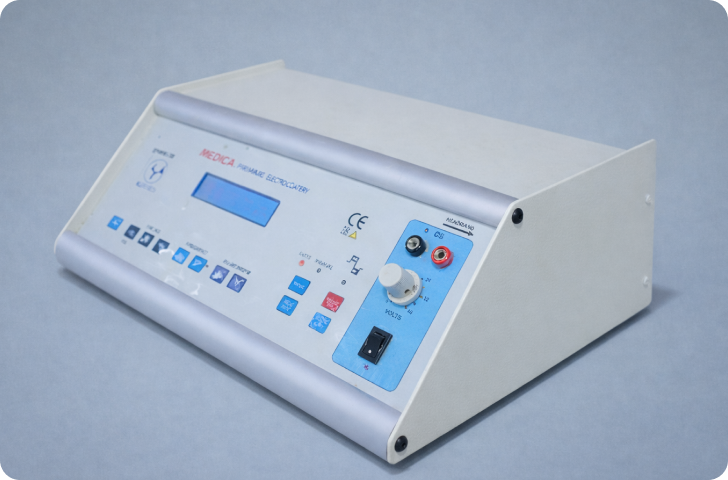
Why ECT is Particularly Effective for Bipolar Disorder:
ECT, also known as Brief Pulse Therapy, is considered the gold standard treatment for severe bipolar disorder, especially when other treatments have been ineffective or when rapid response is critical. At Parth Hospital, we offer the most advanced form of ECT available. ECT is particularly helpful for:
- Severe manic episodes that don't respond to medication
- Severe depressive episodes, especially with suicidal thoughts
- Mixed episodes with significant distress
- Situations where rapid symptom improvement is essential
- Pregnant patients for whom medications may pose risks
- Patients who cannot tolerate medications
Our ECT Safety Record: We’re proud of our perfect safety record across 3,000+ ECT sessions. We use state-of-the-art equipment and protocols that prioritise both effectiveness and patient comfort.
What to Expect:
- Administered under anaesthesia, so you're completely comfortable
- The procedure takes only a few minutes
- Usually performed 2-3 times per week
- Most patients need 6-12 sessions for optimal results
- Side effects are minimal with modern techniques
Specialized Expertise
Dr. Parth Goyal is Yale-trained in advanced neurostimulation and specializes in evidence-based bipolar disorder treatment.
Comprehensive Treatment Options
We offer ECT, rTMS, long-acting injectables (LAIs), and ketamine therapy—all under one roof.
Safety and Quality
Our perfect safety record across 2,000+ ECT sessions reflects our unwavering commitment to patient care.
Advanced Technology
We use cutting-edge ECT equipment and were first in Ahmedabad to offer Deep TMS for innovative treatment.
Individualized Care
Your treatment plan is carefully tailored to your specific symptoms, needs, and goals.
Compassionate Approach
We treat every patient with care and respect—mental health treatment should never feel impersonal.
Accessible Care
Through Mind Wellness Charitable Trust, we make psychiatric care accessible regardless of financial circumstances.
Proven Outcomes
Our evidence-based protocols consistently deliver positive results and improved quality of life.
Holistic Support
We provide family education, crisis planning, and ongoing support throughout your recovery journey.
Living Well with Bipolar Disorder
With proper treatment and support, individuals with bipolar disorder can lead fulfilling, productive lives. Recovery is possible, and many people with bipolar disorder achieve long-term stability.
Common medication categories include:
- Consistent medication adherence and regular follow-up appointments
- Healthy sleep habits and maintaining regular routines
- Stress management techniques and building a strong support network
- Avoiding alcohol and recreational drugs
- Recognizing early warning signs of mood episodes
Support for Families
Bipolar disorder impacts the entire family. We provide education and support to help families navigate the condition and care for their loved ones.
Family Resources Include:
- Educational sessions about bipolar disorder, symptoms, and treatment options
- Communication strategies for effective dialogue and expressing concerns supportively
- Crisis management planning, identifying warning signs, and emergency protocols
- Coping skills for caregivers to manage stress and prevent burnout
- Support group connections for shared experiences and mutual encouragement
FAQs
Is bipolar disorder curable?
While bipolar disorder is a lifelong condition, it is highly treatable. With proper treatment and management, most people with bipolar disorder can achieve significant symptom control and lead fulfilling lives.
How long does treatment take?
Bipolar disorder requires ongoing management. Initial stabilization may take several weeks to months, but long-term treatment is essential to prevent relapse and maintain stability.
Is ECT safe?
Modern ECT is extremely safe. At Parth Hospital, we’ve maintained a perfect safety record across 2,000+ sessions. Side effects are minimal with contemporary techniques, and the treatment is performed under anesthesia for maximum comfort.
Can I stop medication once I feel better?
No. Stopping medication when you feel better is one of the most common reasons for relapse. It’s essential to continue treatment as prescribed, even when symptoms are controlled.
How do I know if I need hospitalization?
If you’re experiencing severe symptoms that impair your ability to care for yourself, pose a risk to yourself or others, or haven’t responded to outpatient treatment, inpatient care may be appropriate. Contact us for an assessment.
Does insurance cover bipolar disorder treatment?
Many insurance plans cover psychiatric treatment. We recommend contacting your insurance provider to understand your coverage. We also offer self-pay options and work with the Mind Wellness Charitable Trust to provide accessible care.
An interactive infographic explaining bipolar disorder symptoms, types, and treatment options through clear visuals and easy-to-understand information