- Home
- >
- Electroconvulsive Therapy (ECT)
Advanced Brief Pulse Therapy: The Gold Standard in Psychiatric Care
Brief Pulse Therapy (BPT) is the modern form of (ECT), using narrow electrical pulses under anesthesia. Considered the gold standard for psychiatric treatment, Parth Hospital delivers BPT with advanced equipment and strict protocols.
For many years, cinematic portrayals of ECT have misrepresented a necessary medical procedure.
ECT has often been shown as:

These depictions are medically inaccurate and have contributed to widespread fear and misunderstanding.
Such portrayals have led many people to view ECT as a last-resort punishment rather than a scientifically validated medical treatment.
One of the few mainstream portrayals that accurately reflected modern ECT was in the TV series Homeland, where the procedure was shown being used for Bipolar Mood Disorder under medical supervision.
Several clinicians and researchers have addressed this misinformation through scientific publications and public discourse, with the aim of de-stigmatising ECT so that patients who need it do not avoid care due to fear.
ECT may be recommended in the following psychiatric conditions
Schizophrenia & Allied Psychotic Conditions
(Includes delusional disorders and first-episode psychosis)
Major Depressive Disorder
Suicidal Tendencies Arising from Mental Disorders
Violent or Aggressive Behaviour Resulting From Psychiatric Illness
Bipolar Mood Disorder
Mania
Catatonia
Neuroleptic Malignant Syndrome
Situations Where Reducing Hospital Stay is Clinically Beneficial
At Parth Hospital, our psychiatry services combine clinical expertise, compassionate care, and evidence-based interventions to manage mental health conditions across all age groups
ECT can be administered as both:
When Done as an OPD Procedure:
The Decision Between OPD and IPD is Based on:
ECT involves the application of controlled electrical stimulation to the brain for a very brief duration (typically 1–3 seconds).
- Reduction in overall disease burden
- Improvement in psychiatric symptoms
- Better responsiveness to ongoing medications
Before administering BPT, a thorough pre-ECT workup is carried out to minimise anaesthesia-related and medical risks. Investigations may include:
Complete Blood Count (CBC)
Serum Electrolytes
Serum Creatinine
Liver Function Tests (SGPT)
ECG
Chest X-ray (If Respiratory Illness is Suspected)
CT Scan or MRI brain (If Clinically Required)
Fasting Requirements
Patients are advised to have NO SOLID INTAKE and NO LIQUID INTAKE (INCLUDING WATER) for 3–4 HOURS BEFORE the procedure.
What Happens During the Procedure?
During BPT:
- The patient is brought on an empty stomach
- A trained anesthesiologist administers a short-acting anesthetic agent (Typical duration: 10–12 minutes)
- A muscle relaxant is given to relax the entire body
- Electrical stimulation is delivered for 1–3 seconds
- A therapeutic seizure is elicited and monitored
- The patient regains consciousness after anesthesia wears off
- Once stable, the patient is discharged
Throughout the procedure:
Emergency medications are always kept ready to manage any complication, should it arise.
ECT at Parth Hospital is supported by dedicated equipment, including:
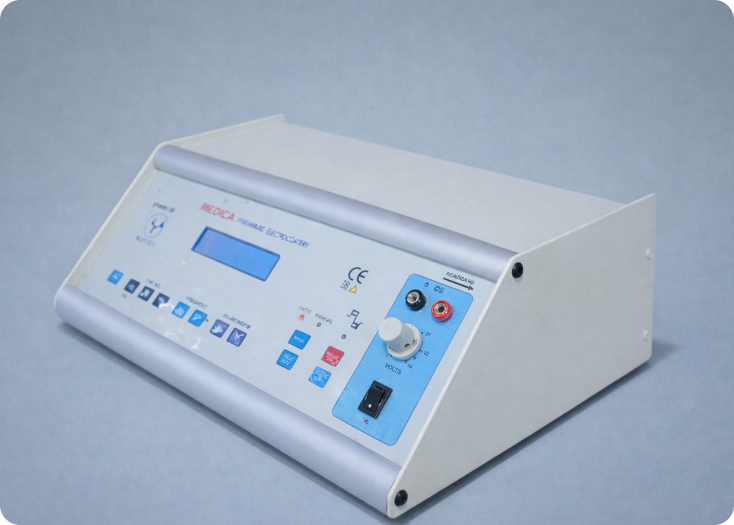
BPT Machine (RMS PC-ECTON Brief Pulse Therapy Machine)
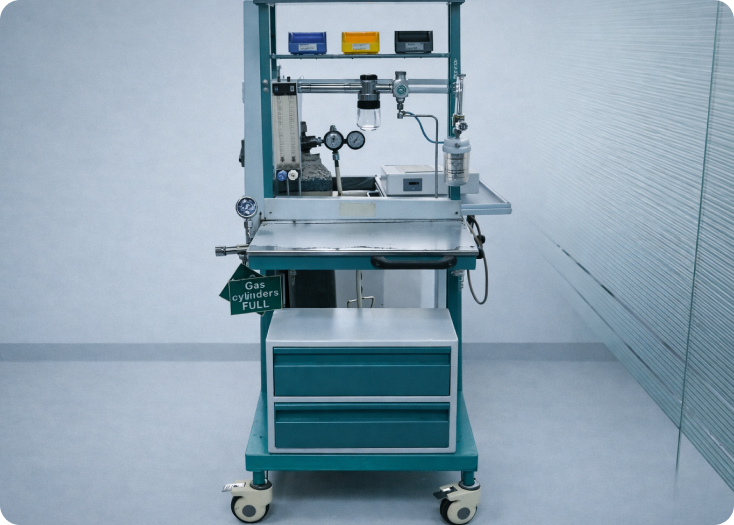
Boyle’s Apparatus and Anaesthetic Trolley

Multi-Parameter Monitor (Philips MP-5)

BPL Monophasic Defibrillatorr
This infrastructure ensures:
Myths vs Facts
| MYTH | FACTS |
|---|---|
|
|
|
|
|
|
|
|
|
|
|
|
Probable Side Effects after BPT
Some Patients May Experience:
Common Post-BPT Side Effects Include:
Memory Disturbances, if Present, Usually:
When Should ECT Be Chosen?
ECT may be considered when patients experience:
- Melancholic Major Depressive Disorder (MDD)
- Major Depressive Disorder (MDD) with psychosis
- Severe aggression or irritability
- Persistent feelings of hopelessness or worthlessness
- Severe slowing of thoughts and actions
- Residual symptoms not responding to medications
- Complete social isolation and poor functioning
- Reduced appetite
- Suicidal thoughts, actions, or attempts

A prior good response to ECT is also an important deciding factor.
Role in Reducing Disease Burden & Long-Term Outcomes

By reducing the overall disease burden, ECT:
- Improves symptom control
- Enhances the effectiveness of medications
- Reduces the need for higher medication doses
- Supports faster functional recovery
- Decreases hospitalization duration and frequency
- Minimizes risk of relapse and recurrence
- Improves quality of life and daily functioning
- Reduces suicidal ideation and self-harm risk
- Enhances cognitive function in severe Major Depressive Disorder (MDD)
FAQs
Is ECT painful, and will I be awake during the procedure?
No, ECT is not painful, and you will not be awake. The procedure is performed under general anesthesia administered by a trained anesthesiologist, so you’re completely unconscious and feel nothing during treatment. A muscle relaxant is also given to relax your entire body. The electrical stimulation itself lasts only 1–3 seconds. You regain consciousness after the anesthesia wears off, typically within 10–12 minutes total procedure time.
Will ECT cause permanent memory loss or brain damage?
No. ECT does not cause permanent memory loss or brain damage. Some patients may experience temporary confusion or short-term forgetfulness after treatment, but these memory disturbances, if present, are self-limiting—usually lasting a few hours and occasionally up to 21 days. They resolve on their own without requiring additional medications. ECT causes biochemical changes in the brain that help reduce symptoms, not structural damage.
When is ECT recommended instead of just continuing with medications?
ECT may be recommended for several psychiatric conditions including severe depression (especially with psychotic features or suicidal thoughts), schizophrenia, bipolar disorder, catatonia, or when there’s severe aggression or violent behavior. It’s particularly considered when patients experience residual symptoms not responding to medications, complete social isolation and poor functioning, or when rapid symptom improvement is clinically necessary. A prior good response to ECT is also an important deciding factor.
Can ECT be done as an outpatient procedure, or does it require hospitalization?
ECT can be administered both as an outpatient (OPD) or inpatient (IPD) procedure. When done as outpatient treatment, admission is not required—you arrive at the scheduled time and are discharged a few hours after the procedure once stable. The decision between OPD and IPD is based on clinical severity, medical stability, and need for close monitoring. This flexibility makes treatment more accessible.
How does ECT actually help improve psychiatric symptoms?
ECT involves controlled electrical stimulation to the brain for 1–3 seconds, which produces a therapeutic seizure. This leads to reduction in overall disease burden, improvement in psychiatric symptoms, and better responsiveness to ongoing medications. By reducing the disease burden, ECT improves symptom control, enhances medication effectiveness, reduces the need for higher medication doses, and supports faster functional recovery. It works through biochemical changes that help restore brain function.
Scientific References
Evidence-based research supporting our clinical approach
Slotema CW, Blom JD, Hoek HW, Sommer IE. Should we expand the toolbox of psychiatric treatment methods to include Repetitive Transcranial Magnetic Stimulation (rTMS)? A meta-analysis of the efficacy of rTMS in psychiatric disorders. J Clin Psychiatry 2010; 71:873.
Liu B, Zhang Y, Zhang L, Li L. Repetitive transcranial magnetic stimulation as an augmentative strategy for treatment-resistant depression, a meta-analysis of randomized, double-blind and sham-controlled study. BMC Psychiatry 2014; 14:342.
Berlim MT, Van den Eynde F, Daskalakis ZJ. High-frequency repetitive transcranial magnetic stimulation accelerates and enhances the clinical response to antidepressants in major depression: a meta-analysis of randomized, double-blind, and sham-controlled trials. J Clin Psychiatry 2013; 74:e122