The Hardest Decision a Parent Must Make
Rajesh sits in his automobile outside Parth Hospital, hands tightening around the steering wheel. His 22-year-old son Arjun sits silently gazing out the window—as he has for weeks.
Two years of outpatient treatment. Six medications. Sleepless nights running into thousands have brought him to this point.
“I felt as if I was failing as a father,” says Rajesh. “But watching your child disappear before your eyes… sometimes love means making the hardest choice.”
If you’re struggling with this impossible choice—this guide is for you.
Understanding what clinical depression really means →
When Outpatient Care Isn’t Enough
Think of mental health treatment like a toolbox:
| Outpatient Tools | When You Need Inpatient Care |
|---|---|
| Weekly therapy sessions | 24/7 medical monitoring required |
| Daily medication at home | Intensive therapy (multiple daily sessions) |
| Family support | Safety-controlled environment |
| Crisis hotlines | Full treatment team coordination |
| Regular psychiatrist visits | Advanced interventions (ECT, TMS, ketamine) |
Learn about advanced treatment options like rTMS →
Deep TMS for treatment-resistant depression →
The Warning Signs: When Rajesh Knew
Arjun’s decline over 24 months:
| Timeline | Symptoms | Crisis Point |
|---|---|---|
| Months 1–12 | Occasional sad days, some withdrawal | Manageable with outpatient |
| Months 13–18 | Missing work regularly, lost interest in friends | Concerning but trying harder |
| Months 19–24 | Stopped leaving room, day/night reversed | Outpatient failing |
| Crisis | Suicidal thoughts, stopped eating, refused contact | Immediate action needed |
Read: What causes depression – internal or external factors? →
Early on, Arjun’s symptoms looked like typical stress. But depression is more than just sadness—it’s a medical condition affecting brain chemistry.
Understanding the warning signs of declining mental health →
Red Flags Requiring Immediate Help
When Rajesh made the decision:
- Suicidal statements: “I wish I could just disappear”
- Complete self-care breakdown: Not eating, bathing, or basic hygiene
- Total isolation: Refusing all human contact
- Reality distortion: Hopelessness as absolute unchangeable fact
- Family fear: Parents afraid to leave him alone
Arjun’s extreme exhaustion wasn’t laziness—it was a symptom of severe depression affecting his brain’s ability to function.
Why depression makes you extremely tired and fatigued →
Crisis Resources (Keep These Numbers Handy)
Immediate Help:
- KIRAN Mental Health Helpline: 1800-599-0019 (24/7)
- Emergency: Go to nearest hospital emergency room
- Parth Hospital Crisis Line: [Number for immediate evaluation]
What Actually Happens: Day 1
Rajesh’s experience of admission:
| Hour | What Happened | Rajesh’s Feelings |
|---|---|---|
| Hour 1 | Welcomed by patient coordinator (not security), comfortable consultation room | Apprehensive but relieved—this feels like healthcare, not punishment |
| Hour 2–3 | Mental health & physical assessment, review of medication, interview of family | Heard and understood—finally in months |
| Hour 4 | Treatment plan discussed, room allocated, family schedule set | Hesitantly hopeful—professionals in charge |
“First time in two years, I wasn’t alone in this. A whole team was now working with Arjun.”
Modern psychiatric care has evolved significantly. Healthcare is becoming more accessible and patient-centered than ever before.
Learn about mental health services →
What It’s Actually Like: Not a Prison
Common fears vs. reality:
| Fear | Reality at Modern Facilities |
|---|---|
| “It’s like a prison” | Private rooms, easy-to-navigate common areas, patient dignity respected |
| “He’ll be sedated like a zombie” | Medication carefully calibrated for active participation in therapy |
| “Other patients will be dangerous” | Patients sorted by age/acuity, rigorous safety protocols |
| “It will ruin his future” | Protected health information, many successful individuals use inpatient care |
One of Rajesh’s biggest concerns was medication. He’d heard so many myths about psychiatric drugs.
Read: 9 myths about psychiatric medication debunked →
The reality? Psychiatric medications, when properly prescribed and monitored, help restore normal brain chemistry—similar to how insulin helps regulate blood sugar in diabetes.
The Treatment Process: Week by Week
Arjun’s 4-week recovery process:
| Week | Focus | Arjun’s Progress | Family Experience |
|---|---|---|---|
| Week 1 | Crisis stabilization | Slept 16 hrs/day, not much talking | Learned about depression biology |
| Week 2 | Engagement building | Had first go at group, smiled at a joke | Learned new communication strategies |
| Week 3 | Skill development | Led group, made friends | Family therapy without tears (first time!) |
| Week 4 | Real-world prep | Day spent home, came back voluntarily | Had sense of being prepared to support recovery |
Key insight: Recovery occurs in stages, not immediately. Progress is evident in tiny moments before dramatic changes.
During Week 2, Arjun began processing some childhood experiences that contributed to his depression. Understanding the root causes helped him make sense of his struggles.
Understanding what triggers depression →
The family also learned crucial skills. The way family members communicate can significantly impact recovery outcomes.
How family support affects mental health recovery →
Why 24/7 Care Matters
The broken bone metaphor:
| Treatment Type | Comparison |
|---|---|
| Outpatient care | Physical therapy while walking on broken leg |
| Inpatient care | Setting the bone correctly before rehab |
| Intensive treatment | Surgery that corrects underlying damage |
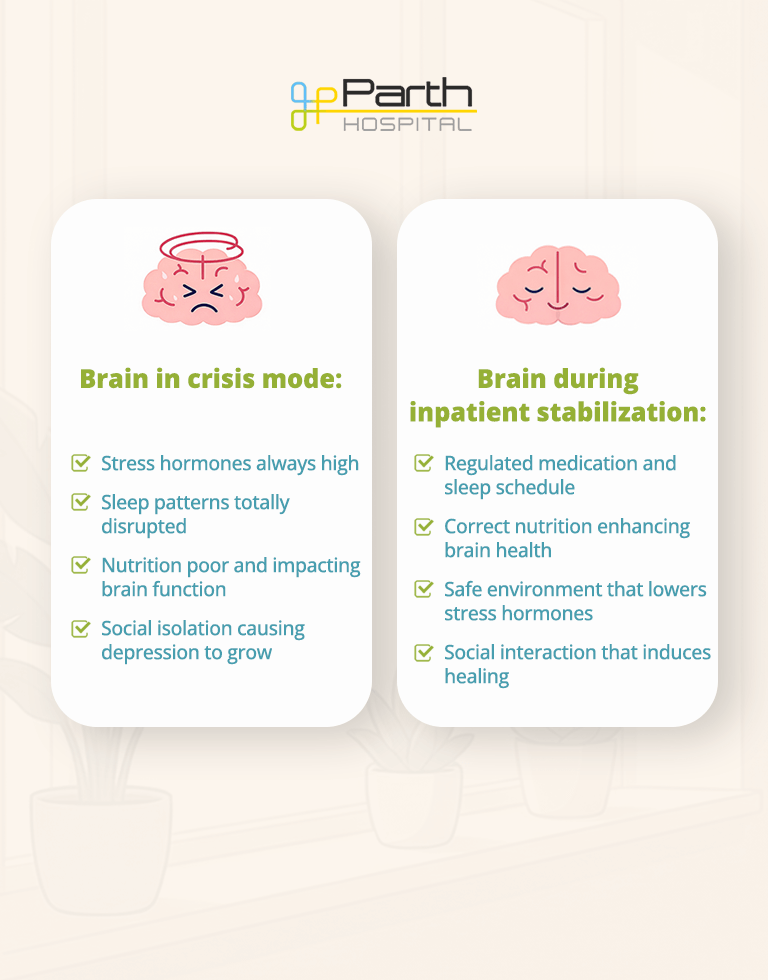
Brain in crisis mode:
- Stress hormones always high
- Sleep patterns totally disrupted
- Nutrition poor and impacting brain function
- Social isolation causing depression to grow
Brain during inpatient stabilization:
- Regulated medication and sleep schedule
- Correct nutrition enhancing brain health
- Safe environment that lowers stress hormones
- Social interaction that induces healing
Learn about Psychotherapy & Counselling services →
Understanding Other Conditions
While Arjun’s diagnosis was severe depression, inpatient care treats many conditions:
Depression and mood disorders – When symptoms become life-threatening or completely disable daily functioning
What is clinical depression? →
Anxiety disorders – When panic attacks, obsessions, or phobias prevent normal life
Understanding anxiety disorders →
OCD myths and facts →
Psychotic episodes – When someone loses touch with reality through hallucinations or delusions
What are hallucinations in mental illness? →
Addiction and substance abuse – When dependencies become dangerous to health and safety
De-addiction treatment options →
The Financial Reality
Cost factors:
| Factor | Typical Range (India) |
|---|---|
| Average stay | 7–28 days |
| Total cost | ₹2–8 lakhs (full treatment) |
| Includes | Room, meals, all therapy, medications, discharge planning |
Cost of NOT receiving inpatient care:
- Several ER visits: ₹5,000-10,000 per visit
- Lost wages: Patient can’t work months/years
- Family implication: Parents missing work
- Multiple failed outpatient attempts
- Worst-case scenarios: Unmeasurable costs
Insurance: Mental health parity legislation mandates equal coverage. Payment plans and financial aid offered.
Making the Decision: When It’s Right
Ask yourself:
Safety:
- Thoughts of suicide or harming self?
- Stopped taking basic care of self?
- Scared to leave them alone?
Treatment effectiveness:
- Outpatient treatments not working?
- Can’t attend therapy?
- Symptoms getting worse despite therapy?
Daily functioning:
- Can’t work, go to school, or have relationships?
- Totally isolated?
- Can’t make decisions about care?
- Family in crisis holding together?
If you said YES to more than one of these questions—inpatient care should be seriously considered.
Sometimes recognizing the warning signs early can prevent a full crisis.
Warning signs your mental health may be declining →
What Happens Next
Admission process:
- Call hospital for consultation
- Initial evaluation appointment
- Psychiatric assessment
- Treatment recommendation
- Family decision meeting
- Scheduling of admission if warranted
Keep in mind: Early intervention produces improved results. The most difficult choice may be the most life-saving.
🏥 Parth Hospital Ahmedabad
Inpatient & Emergency Psychiatric Services
📍 Address: 3rd Floor Sigma Excellence, Near Management Enclave, Opposite Falguni Gruh Udyog, Vastrapur, Ahmedabad, 380015
📞 24/7 Emergency Contact:
- (+91) 972 420 1332
- (+91) 987 972 5516
📧 Email: info@parthhospital.com
🕐 Consultation Hours:
Monday – Saturday
Morning: 9:00 AM – 1:00 PM
Evening: 4:00 PM – 7:00 PM
🆘 In case of crisis in your loved one, call Parth Hospital Ahmedabad for urgent assessment.
The crisis is short-lived. Recovery is attainable. Support is at hand.
📋 MEDICAL DISCLAIMER
This content is for educational purposes only and does not constitute medical advice. Decisions about inpatient psychiatric care should be made in consultation with qualified mental health professionals who can assess the individual’s specific situation. Every case is unique and requires professional evaluation.
If you’re concerned about a loved one’s mental health, contact a mental health professional or crisis service immediately for proper assessment and guidance.